Renaud Govoetchan, Mohamed Mousse Ibrahim, Arthur Sovi, Houssein Mouhamed Omar, Abdillahi Omar Boulhan, and Houssein Youssouf Darar from the different institute of the Benin an UK, wrote a research article about Anopheles stephensi: Malaria's New Threat in Djibouti, entitled "Anopheles stephensi: The emerging vector of malaria in the Republic of Djibouti, Horn of Africa." This research paper published by the International Journal of Biosciences | IJB an open access scholarly research journal on Biology, under the affiliation of the International Network For Natural Sciences | INNSpub, an open access multidisciplinary research journal publisher.
Abstract
The present study
investigated mosquito species composition and phenotypic insecticide resistance
profile to support decision-making in vector control in the Republic of
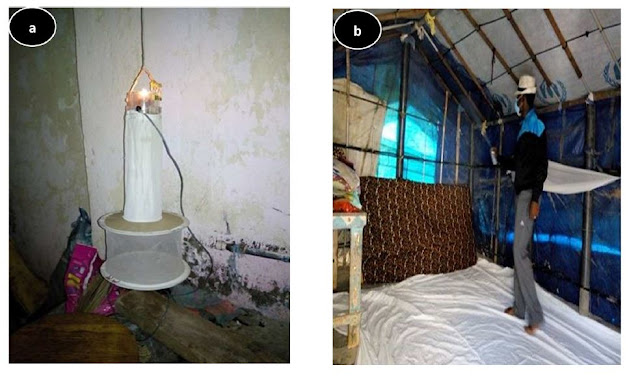
Djibouti at the Horn of Africa. Adult mosquitoes were collected between
December 2016 and December 2017 across 20 sentinel sites established in the 6
regions of the country using both Centers for Disease Control (CDC) miniature
light traps and pyrethrum spray catches (PSC). Female mosquitoes were kept aside,
for morphological identification to species by an expert entomologist using
appropriate taxonomic keys by Gillies & Coetzee and Glick. Bioassays were
also conducted in An. stephensi from Djibouti-ville against nine
insecticides used in public health. A total number of 12,538 host-seeking
mosquitoes belonging to four genera (Anopheles, Culex, Aedes, Uranotaenia)
comprising 12 species were collected. Among these, A. gambiae S.L.
and A. stephensi were the two major malaria vectors identified while
secondary malaria vectors such as A. nili somalicus, A. dthali and A.
azaniae were also collected. Culex quinquefasciatus was the most
abundant mosquito species in the 6 regions. WHO susceptibility tests performed
on A. stephensi population from Djibouti-ville showed resistance to
pyrethroids, organophosphates, carbamates and DDT. The resistance intensity
bioassays indicated low to moderate intensity of resistance with pyrethroid
insecticides and the organophosphate pirimiphos methyl. Meanwhile pre-exposure
to PBO suggested involvement of P450 detoxification enzymes in pyrethroid
resistance. These findings revealed the urgent need to develop and implement a
programme for monitoring and managing insecticide resistance in local vector
populations with efficient control strategies in Djibouti.
Read more: Dengue Epidemiology: Seasonal Trends in Tangub City | InformativeBD
Introduction
Located in the Horn of Africa, the Republic of Djibouti shares borders with Eritrea, Ethiopia and Somalia and has just over 300 km of coastline along the Red Sea and Gulf of Aden (Hatem, 1996). With an area of 23,200km2 consisting mainly of plateau, plains and highlands, the Republic of Djibouti has a hot and humid climate, with a temperature that varies between 30°C in January and 43°C in July with an average humidity of 69% (Schulman, 2019).
Rainfall is rare (<130mm annually), however unusual rains may occur across the country causing heavy rainfall and flooding in residential areas of the capital Djibouti-ville (Schulman, 2019). In the Republic of Djibouti, mosquito-borne diseases are primarily transmitted by malaria vectors and secondarily dengue fever vectors, followed by other diseases with suspected cases such as West Nile virus and Leishmaniasis (Faulde et al., 2012; Rodier, 1995). While the Horn of Africa is known to be highly susceptible to mosquito-borne diseases, the Republic of Djibouti was historically thought to be a malaria meso to hypo-endemic country with intermittent epidemics (Rodier, 1995). However local populations have experienced only low and unstable malaria transmission and intermittent epidemics (Fox et al., 1991; Fox et al., 1989) with most of cases detected in people returning from neighbouring countries (Khaireh et al., 2013; Crowell et al., 2012).
The first case of malaria was reported at the very beginning of the 20th century, but it was not common until 1984 that malaria became a public health problem after a significant number of imported malaria cases were recorded. Since then, malaria cases have continued to increase, most importantly in Djibouti-ville. From 1988, there was an increase in malaria cases throughout the country, even in the regions of Tadjourah and Obock that were not affected in the past. In order to address the progression of the disease, the country implemented its first vector control programs based initially on larval control (Louis, 1988; Carteron et al., 1979) strengthened later with the introduction of insecticide-treated bed nets.
Unfortunately, investments and control efforts did not commensurate with the risks of disease, and major malaria outbreaks were reported. In 1991, a record of 7,338 microscopically confirmed malaria cases declining to 4,770 cases in 1993 (Rodier, 1995).
Contrastingly, an unusual increase of malaria cases was reported in 1999 in and around Djibouti-ville due to the emergence of chloroquine resistance (Rogier et al., 2011). The cases detected were mainly caused by Plasmodium falciparum but also P. vivax which was responsible of 3% of malaria burden (UNDP, 2013).The last uncommon urban outbreak of malaria was observed in 2013 with 1228 reported cases of which 83% were from Djibouti-ville alone (UNDP, 2013).
The entomological surveillance in Republic of Djibouti was not a routine exercise and as such the monitoring programme at country level is very poor. Most of the existing data were generated as part of the international European Union Naval Force Somalia mission “Atalanta” (Faulde et al., 2012; Faulde & Ahmed, 2010) by the country's military partners that have troops based at various locations throughout the territory. The local malaria transmission was attributed to Anopheles arabiensis in all the 6 regions of the country (WHO, 2012).
However, a larval survey has reported the presence of A. nili in Ali Sabieh, southern region of Djibouti. More recently, A. stephensi, the Asian malaria mosquito vector of Plasmodium falciparum and P. vivax was incriminated in the outbreak which occurred in 2013 (Faulde et al., 2014).
The current study updates malaria entomological data mandatory for decision making on control strategies implementation. The data was generated over a recent entomological surveillance conducted between December 2016 and December 2017, in 20 sentinel sites located along the south-north transect of Djibouti Republic. Mosquito species compositions, as well as insecticide resistance status of the main malaria vector identified in the Djibouti-ville were assessed to support decision-making for the implementation of an efficient control program.
Reference
Ahmed A. 2021.
Invasive Malaria Vector Anopheles stephensi Mosquitoes in Sudan,
2016-2018. Emerg Infect Dis 27(11), 2952-2954.
Ali S. 2022.
Morphological identification and genetic characterization of Anopheles
stephensi in Somaliland. Parasit Vectors 15(1), 247.
Carteron B, Morvan D,
Rodhain F. 1979. The control of culicidae in Djibouti town. An experience
of 7 years (Author’s transl)]. Med Trop 39(5), 555-8.
Corbel V, Chabi J,
Dabiré RK, Etang J, Nwane P, Pigeon O, Hougard JM. 2010. Field efficacy of
a new mosaic long-lasting mosquito net (PermaNet® 3.0) against
pyrethroid-resistant malaria vectors: A multi centre study in Western and
Central Africa. Malaria Journal 9(1), 1-12.
Crowell VHD, Briët O,
Chitnis N, Maire N, Smith T. 2012. Can we depend on case management to
prevent re-establishment of P. falciparum malaria, after local
interruption of transmission. Epidemics 4, 1-8.
de Santi VP. 2021.
Role of Anopheles stephensi Mosquitoes in Malaria Outbreak, Djibouti, 2019.
Emerg Infect Dis 27(6), 1697-1700.
Enayati A. 2020.
Evolution of insecticide resistance and its mechanisms in Anopheles
stephensi in the WHO Eastern Mediterranean Region. Malar J 19(1), 258.
Faulde MK, Rueda LM,
Khaireh BA. 2014. First record of the Asian malaria vector Anopheles
stephensi and its possible role in the resurgence of malaria in Djibouti,
Horn of Africa. Acta Trop 139, 39-43.
Faulde MK, Spiesberger
M, Abbas B. 2012. Sentinel-site-enhanced near-real time surveillance
documenting West Nile virus circulation in two Culex mosquito species
indicating different transmission characteristics, Djibouti City, Djibouti. J.
Egypt. Soc. Parasitol 42, 281-294.
Faulde MK, Ahmed
AA. 2010. Haematophageous vector monitoring in Djibouti city from 2008 to
2009: first records of Culex pipiens ssp. torridus (IGLISCH),
and Anopheles sergentii (Theobald). J Egypt Soc Parasitol, 40(2), 281-94.
Fox E, Abbate EA, Leef
M, Mikhail E, Said-Salah Y, Hassan A. 1989. Malaria in the Djibouti
Republic: Results of a serologic survey in Ambouli. Med. Trop 51, 185-189.
Fox E, Bouloumie J,
Olson JG, Tible D, Lluberas M, Shakib SO, Parra JP, Rodier G. 1991. Plasmodium
falciparum voyage en train d’Éthiopie à Djibouti. Med. Trop 51, 185-189.
Ghosh SK. 2020. Anopheles (Cellia)
stephensi Liston 1901: the vector of urban malaria- An imminent threat to
malaria elimination in India. In: Vector Biology and Control, an update for
malaria elimination initiative in India (Dev V, Editor), The National Academy
of Sciences, India pp. 69-82.
Gorouhi MA. 2016.
Current Susceptibility Status of Anopheles stephensi (Diptera:
Culicidae) to Different Imagicides in a Malarious Area, Southeastern of Iran.
J. Arthropod Borne Dis 10(4), 493-500.
Gillies MT, Coetzee
M. 1987. A supplement to the Anophelinae of Africa South of the Sahara.
Publ S Afr Inst Med Res 55, 1-143.
Glick JI. 1992.
Illustrated key to the female Anopheles of southwestern Asia and
Egypt (Diptera: Culicidae). Mosq Syst 24, 125-153.
Hatemmm. 1996.
Health development in Djibouti. World Health Forum 17(4), 390-1.
Hemingway J, Ranson H. 2020.
Insecticide resistance in insect vectors of human disease. Annual review of
entomology 45(1), 371-391.
Khaireh BA. 2013.
Population genetics analysis during the elimination process of Plasmodium
falciparum in Djibouti. Malar J 12, 201.
Louis JP. 1988.
Malaria in the Republic of Djibouti. Strategy for control using a biological
antilarval campaign: Indigenous larvivorous fishes (Aphanius dispar) and
bacterial toxins. Med Trop 48, 127-131.
Ngongang-Yipmo ES. 2022.
Reduced performance of community bednets against pyrethroid-resistant Anopheles
funestus and Anopheles gambiae, major malaria vectors in Cameroon.
Parasit Vectors 15(1), 230.
Nkemngo FN. 2020.
Multiple insecticide resistance and Plasmodium infection in the
principal malaria vectors Anopheles funestus and Anopheles
gambiae in a forested locality close to the Yaounde airport, Cameroon.
Wellcome Open Res 5, 146.
Oliver SV, Lyons CL,
Brooke BD. 2022. The effect of blood feeding on insecticide resistance intensity
and adult longevity in the major malaria vector Anopheles funestus (Diptera:
Culicidae). Sci Rep 12(1), 3877.
Pinda PG. 2020.
Comparative assessment of insecticide resistance phenotypes in two major
malaria vectors, Anopheles funestus and Anopheles arabiensis in
south-eastern Tanzania. Malar J 19(1), 408.
Ranson H, Lissenden N. 2016.
Insecticide resistance in African Anopheles mosquitoes: A worsening
situation that needs urgent action to maintain malaria control. Trends in
Parasitology 32(2), 187-196.
Rodier GR. 1995.
Recurrence and emergence of infectious diseases in Djibouti city. Bull World
Health Organ 73(6), 755-9.
Rogier C. 2005.
Malaria epidemic and drug resistance, Djibouti. Emerg Infect Dis 11(2), 317-21.
Safi NH. 2017.
Evidence of metabolic mechanisms playing a role in multiple insecticides
resistance in Anopheles stephensi populations from Afghanistan. Malar
J 16(1), 100.
Sanou A, Nelli L,
Guelbéogo WM, Cissé F, Tapsoba M, Ouédraogo P, Ferguson HM. 2021.
Insecticide resistance and behavioural adaptation as a response to long-lasting
insecticidal net deployment in malaria vectors in the Cascades region of
Burkina Faso. Scientific reports 11(1), 1-14.
Schulman S. 2019.
Climate Change Challenges and Djibouti. The RUSI Journal 164(1), p.
62-75.
Seyfarth M. 2019.
Five years following first detection of Anopheles stephensi (Diptera:
Culicidae) in Djibouti, Horn of Africa: populations established malaria
emerging. Parasitol Res 118(3), 725-732.
Simpson EH. 1949.
Measurement of Diversity. Nature 163, 688-688.
Singh OPDC, Lather M,
Agrawal OP, Adak T. 2011. Knockdown resistance (kdr)-like mutations in the
voltage-gated sodium channel of a malaria vector Anopheles stephensi and
PCR assays for their detection. Malar Journal 10(59).
Takken W, Lindsay S. 2019.
Increased Threat of Urban Malaria from Anopheles stephensi Mosquitoes,
Africa. Emerg Infect Dis 25(7), 1431-1433.
United Nations
Developement Programme. 2013. Djibouti: Appel Global–Revue à mi-Parcours.
WHO. 2012. World
malaria report 2011. 2012.
WHO. 2016. Test
procedures for insecticide resistance monitoring in malaria vector mosquitoes.
WHO. 2022. WHO
initiative to stop the spread of Anopheles stephensi in Africa.
World Health
Organization. 2012. Global plan for insecticide resistance management in
malaria vectors. World Health Organization.
Yared S. 2020. Insecticide resistance in Anopheles stephensi in Somali Region, eastern Ethiopia. Malar J 19(1), 180.
Source: Anopheles stephensi: The emerging vector of malaria in theRepublic of Djibouti, Horn of Africa









%20in%20full.JPG)


0 comments:
Post a Comment